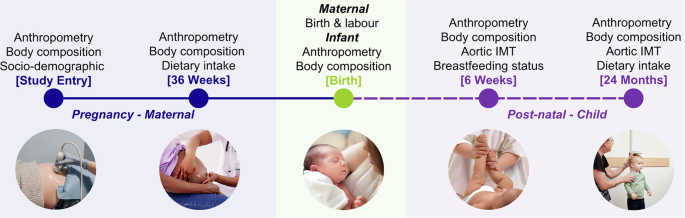
Maternal and child predictors of vascular health in infancy and early childhood
In this sub-study, we found limited evidence that EWG during the first two years of life impacts child vascular health as measured by aIMT. We hypothesise that our lack of findings may be partly due to our sample size, which was impacted by typical attrition in longitudinal studies, as well as attrition and missing data secondary to the COVID-19 pandemic. Additionally, our sample was generally healthy, therefore there were fewer babies born SGA, as a proxy for restricted growth, compared to the population average. Consequently, we were unable to fully test our hypothesis.
Maternal characteristics were associated with infant birthweight and growth velocity, but not aIMT
Approximately half of Australian women have overweight or obesity at the start of pregnancy. High pre-pregnancy weight and BMI is associated with an increased risk of gestational diabetes and foetal macrosomia, both of which are associated with aortic wall thickness in the offspring, albeit in small case-control and cross-sectional studies.32,33 Similarly, in two recent systematic reviews and meta-analyses, the authors found some evidence from small, heterogeneous studies that maternal age and smoking were associated with pre-clinical atherosclerosis in both aortic34 and carotid vascular beds.35 As such, maternal health and wellbeing are of particular interest for the vascular health of the offspring. In this study, we found no associations between maternal determinants and infant aIMT at 6 weeks of age. This aligns with findings by McCloskey et al.13 who found that while maternal pre-pregnancy BMI was positively associated with birthweight, no other maternal factors were associated with either infant growth or aIMT at 6 weeks. Similarly, we observed that measures of maternal adiposity were associated with infant size at birth; specifically, higher early pregnancy weight and gestational weight gain were positively associated with birthweight. Birthweight, in turn, was significantly associated with growth velocity from birth to 6 weeks, with infants born heavier showing slower relative growth in early infancy. This carry-over effect of birthweight on growth trajectory underscores the potential to target maternal health, particularly pre-pregnancy or early pregnancy weight, to influence early infant growth patterns. To that end, most pregnancy interventions have focused on limiting gestational weight gain with offspring birthweight as a secondary outcome. The latest systematic review and meta-analysis evaluating this showed fewer small and large babies with dietary interventions during the antenatal period.36 In terms of preventing growth restriction, there are presently no known interventions.
Interestingly, we found that maternal age was negatively associated with birthweight. This contrasts with the typical positive association between maternal age and birthweight.37 One possible explanation is the unique composition of our cohort: most participants were first-time mothers, and the commonly observed positive association between maternal age and birthweight is often driven by higher parity in older women. Alternatively, the observed negative relationship may reflect an underlying pathological process, as older first-time mothers have a higher risk of placental dysfunction.34
Child growth patterns were not associated with vascular health during early childhood
The prevalence of EWG in full-term children born appropriate for gestational age ranges from 20 to 36%.35 In contrast, up to 80% of infants born premature or with low birthweight experience EWG, although in their case, it is referred to as “catch-up growth”.38 In our study, the prevalence of EWG during early infancy was 26.4%, consistent with previous reports; however, this prevalence increased significantly to 45.3% by 24 months. The discrepancy between our results and those reported in the literature may be attributed to differences in the metrics used to define EWG. While many studies use a change in z-score >0.67 SD as the threshold, the specific z-score applied, such as weight, BMI, or weight-for-length, varies. Additionally, the timeframes assessed, such as 0–12 months or the first two years, differ between studies. In this study, we used the change in weight-for-length/height z-scores. This method has been used before5 and allows us to account for the changes in weight relative to length. However, when calculating EWG using change in weight z-scores, the prevalence was lower at 6 weeks (12.6%) and 24 months (34.5%). The choice of metric may depend on the specific aim of the study, but it does make establishing the prevalence of EWG and comparisons across studies challenging. Given the study’s small sample, we are hesitant to interpret this finding any further.
Due to the limited sample size (as a pilot study) and the overall healthy population, we were unable to specifically explore the impact of excess postnatal growth in those born SGA. Instead, we explored how significant deviations from a child’s growth trajectory impacted vascular health. We did not find any significant differences in aIMT between those with EWG, decelerated growth, or on-track growth at 6 weeks or 24 months. In our adjusted analysis at 6 weeks, male sex was associated with aIMT. However, as males were larger, longer, and gained more weight than females by 6 weeks, this finding likely reflects inherent differences in size for males. Accordingly, at the 24-month follow-up, when males and females were comparable in size, we found no association between male sex and aIMT.
Although studies exploring postnatal growth patterns and CVD risk markers are sparse, existing evidence consistently links EWG in infancy with an adverse cardiovascular profile in later life. This includes increased arterial wall thickness in the aortic and carotid vascular beds,5,6 higher blood pressure,5,7,39 higher pulse wave velocity,40 and impaired endothelial dysfunction.41 These biomarkers are associated, at times independently, with an increased risk of future cardiovascular events in adults. EWG in infancy is also linked to the development of childhood obesity and obesity-related risk factors, which may persist into adulthood and predispose individuals to an increased risk for CVD. Recent findings from the Special Turku Coronary Risk Factor Intervention Project, a cohort of 552 individuals followed from early childhood, found that participants with aIMT above the 80th percentile throughout adolescence (ages 11-19) had persistently high BMI from infancy.42 These findings support a mechanism by which early excessive growth may contribute to vascular changes through sustained increases in body size. The study also found that aIMT was more strongly associated with traditional CVD risk factors, such as blood pressure and blood lipids, than carotid IMT, reinforcing our rationale for using aIMT as a marker of early vascular remodelling.
Further granularity is needed to identify the role of maternal and child nutrition on EWG and vascular health
Maternal nutrition plays a crucial role in determining offspring birthweight; however, its influence on infant vascular health is unclear. In a cohort of 201 mother-child dyads, Gale et al.43 demonstrated that low energy intake during early and late gestation was associated with greater carotid IMT in children at nine years of age. Additionally, in a sub-study of a randomised controlled trial examining the benefits of a low-glycaemic index diet compared to a high-fibre diet during pregnancy in high-risk women, Kizirian et al.44 found that offspring in the low-glycaemic index group had significantly lower aIMT at one year of age, but this difference was partly attributed to differences in birthweight between the groups. Conversely, our group has previously not found any relationship between carbohydrate quality and quantity with aIMT45 or cardiac autonomic function,46 nor between fatty acids with aIMT47 in a comparable cohort. However, we have found that the maternal dietary fatty acids influence epigenetic aging49 in the offspring, which could be an indirect mechanism through which maternal diet may influence offspring vascular health and CVD risk. Our study was novel in its attempt to assess child diet in relation to aIMT but we did not find any associations.
In the present study, we did not find any evidence that maternal energy intake and macronutrient distribution affected infant birthweight, growth velocity, or aIMT at 6 weeks. Additionally, no associations were observed between child diet, growth velocity, and aIMT. The lack of observed dietary associations may be attributed to several possibilities: (1) the small sample size inherent to a pilot study, compounded by an even smaller subset with both dietary assessment and aIMT data available, (2) the general non-selected rather than high-risk population, and (3) the use of an FFQ to evaluate diet. In the BABY1000 study, an FFQ was selected to minimise participant burden given the repeated study visits and questionnaires required at each timepoint. Future studies with repeated, prospective measurements of dietary intake are needed to capture detailed nutritional exposures during early life and explore their potential associations with cardiometabolic health.
Strengths and limitations
We consider our study to have several strengths, the first of which is the longitudinal design and collection of a broad range of maternal and child clinical factors, using best practice and validated methodology. Secondly, we used publicly available validated growth standards to characterise size at birth and growth trajectories. The use of standardised growth references can facilitate cross-study comparisons. Lastly, our cohort is broadly representative of women and babies born at RPAH. However, we must acknowledge that this population is primarily English-speaking, tertiary educated, and more affluent, which affects the generalisability of our findings.
Consistent with many prospective and in-depth cohorts, this pilot study has limitations. Firstly, the BABY1000 pilot aimed to assess the feasibility and acceptability of embedding a longitudinal birth cohort study in routine clinical care and was not powered on clinical outcomes. Despite this, the analyses presented here were pre-planned and aligned with the study’s priority questions, formalised in 2016, to explore the relationship between maternal nutrition during pregnancy and offspring cardiometabolic health and to determine the benefits of postnatal nutrition in at-risk groups for cardiometabolic health.15 Secondly, data completeness was significantly impacted by external influences such as the COVID-19 pandemic, public health directives and internal challenges secondary to the pandemic, such as staff efficiency, remote data collection, and a limited study budget. Despite these challenges, there were few differences in those active at baseline and those at follow-up, showing limited bias in our participant retention. Thirdly, not all children who returned for the 24-month follow-up had also attended the 6-week visit, which limited our ability to calculate growth trajectories between the two timepoints. To preserve sample size and maintain statistical power, EWG was defined from birth for each timepoint. While this approach allowed for broader inclusion, it may have obscured timing-specific growth effects during later infancy and early childhood. Additionally, the timing of follow-up visits was influenced by external factors. Ideally, frequent follow-ups, aligned with key growth and developmental milestones, are needed to better characterise growth trajectories during early childhood and their potential relationship with early vascular health.
Lastly, we used two different machines to image aIMT at the two timepoints and two different neonatologists performed the scans. These changes were due to logistical challenges; the examination rooms in the NICU were prioritised for patients undergoing routine health check-ups, limiting their availability for the 24-month follow-up scans, and the availability of the sonographers was affected by patient care needs. We minimised sources of variance in the aIMT measurement by using edge-detection software, which is shown to have greater inter-rater reliability than manual callipers,11 and by having all scans analysed by the same blinded individual with demonstrated reliability. However, future studies should aim to standardise ultrasound equipment and sonographers across timepoints to reduce sources of methodological variance. If the above is not possible, and provided the study is large enough, a sensitivity analysis accounting for the above sources of variance should be done.
link







